It’s a race against time that some participants liken to Apollo 13, the stricken NASA spacecraft for which engineers improvised an air purification system from available parts to get three astronauts back from the moon.
In this case, however, the race is to improvise ventilators, face shields, respirators, surgical gowns, disinfectant wipes, and other healthcare gear to help the hundreds of thousands of people expected to swamp hospitals with waves of critical COVID-19 illness over the next several weeks. The demand for ventilators alone could be four times more than already overwhelmed hospitals can provide.
Using 3D-printed parts, plastic-lined tablecloths intended for birthday parties, laser-cut gears, and similar substitutions, a research team from universities on two continents is racing to develop “do-it-yourself” healthcare gear that can be assembled where it’s needed from components available locally. Team members figure they have about two weeks to get the designs right and share them with anyone who can help with the needs.
“We’re trying to figure out how to get these things to scale in the time we have,” said Shannon Yee, an associate professor in Georgia Tech’s George W. Woodruff School of Mechanical Engineering who’s working on the ventilator issue with a half-dozen colleagues at Georgia Tech and other universities. “We are looking at producing things very quickly and this is where having contacts with mature manufacturing sources is going to help.”
- Georgia Tech has established a Rapid Response website to identify needs for personal protective equipment and potential collaborations.
Supplying Face Shields to the Medical Community
The Wallace H. Coulter Department of Biomedical Engineering at Emory and Georgia Tech serves as a bridge between healthcare needs and the broad technical know-how at Georgia Tech, and Georgia Tech researchers are talking regularly with hospital systems to discuss their needs. So far, hand sanitizer, disinfectant wipes, face shields, respirator masks, and ventilators have been identified as critical needs. Using resources of the Flowers Invention Studio – such as 3D printing – the group has already produced 1,000 face shields and is preparing to fabricate thousands more in the form of kits that hospitals can assemble.
"With the significant challenges on our supply chain, we need strategies to provide personal protective equipment (PPE) for healthcare staff," said Dr. Charles Brown, CEO of Physician Enterprise at Piedmont Healthcare. "We have mechanisms in place to develop ideas and are working with Georgia Tech and the Global Center for Medical Innovation (GCMI) to advance them to what we can use."
Georgia Tech faculty members, students and GCMI worked on multiple face shield designs, talking with clinicians at Children’s Healthcare of Atlanta, Emory Healthcare and Piedmont to evaluate and iterate. The result was two different designs intended for specific uses in hospital facilities, where face shields protect clinicians from splashes and help extend the life of soft respirators intended to filter out virus particles.
“The team has worked hard to identify materials suppliers and define simple and scalable solutions to meet this challenge,” said Sam Graham, chair of the Woodruff School of Mechanical Engineering. “We are fortunate to have partners ready to team up with us to help address some of the shortfalls in medical equipment that hospitals are experiencing."
To scale up fabrication beyond the Georgia Tech campus, the team focused on simple designs that could be shared with and produced by individuals with access to a makerspace – and major manufacturers with injection molding capabilities. The team plans to make the designs available for anyone with laser cutting or 3D printing capabilities.
“Initially we were just thinking about meeting the needs of Atlanta, but cities everywhere need them,” said Saad Bhamla, an assistant professor in the School of Chemical and Biomolecular Engineering who specializes in “frugal science” – creating inexpensive lab devices. “We have created great models that can be used to create a pipeline of instructions that others can use. The face shields will set the stage for other device models as they become available.”
The group is leveraging Georgia Tech contacts with companies to identify suppliers for alternative materials that can go into their “Apollo 13” devices. Team members, including Christopher Saldana, an associate professor in the Woodruff School, are working with GCMI on those issues, using equipment in Georgia Tech’s maker spaces and elsewhere.
"The Georgia Tech mechanical engineering team is working to modify open source face shield designs so they can be manufactured in high volumes for the rapid response environment that COVID-19 requires,” said Christopher Saldana, an associate professor in the Woodruff School. “Our team has modified these designs using a range of product and process optimization methods, including removing certain features and standardizing tool use. By working on cross-functional and cross-disciplinary teams and directly involving healthcare practitioners and high-volume manufacturers, we will be able to respond to this effort at the scale and speed required."
Bringing Georgia Tech’s expertise together to address the challenges – and develop collaborations – has been done behind the scenes by people like Sherry Farrugia, chief operating and strategy officer for the Children’s Healthcare of Atlanta Pediatric Technology Center.
“Serving as kind of a chief strategy officer, my work is to help bridge the gaps, focus the teams, rally the troops, and make critical connections,” she said. “Doing this requires a deep knowledge of who’s doing what on campus, as well as a strong network in the private sector.”
The Supply Chain Challenge
The team is launching a website (www.research.gatech.edu/rapid-response) to both quantify the needs for face shields and solicit supplies of materials. Because the world’s supply chains are unable to ship conventional PPE components, they are looking for alternatives that may not now be part of that production.
The challenge is that everyone is scrambling to find equipment and materials in an international supply chain that has already been depleted by months-long demands from countries that dealt with the virus earlier: China, Italy and South Korea. As the healthcare demands ramp up in the United States, hospitals will have to be more creative in meeting the needs that their traditional sources may not be able to supply.
"Countries on the trailing end of the pandemic are facing supply chain issues that countries with earlier pandemics didn't have to face," said Michael O'Toole, Executive Director of Quality Improvement at Piedmont and a Georgia Tech engineering graduate. "We've got to get these supplies, and its a critical need already. If we can't get them from commercial or government sources, we're going to have to make them ourselves."
With significant efforts going into design of locally sourced equipment, expertise on medical device prototyping and approval is needed. That is coming from a network of alumni and local companies and GCMI, a Georgia Tech-affiliated organization that works with device manufacturers around the world to translate designs into devices that can be manufactured quickly and cost effectively.
“The goal right now is to develop solutions that can be sourced locally and that we can produce now,” said Tiffany Wilson, GCMI’s CEO. “We are working with Georgia Tech and others on how we can suggest modifying the designs to optimize them for the current environment. We are helping make sure designs are clinically validated with an eye toward scalability.”
Beyond its experience with medical devices, GCMI is also helping source materials and components, and working with regulators at the FDA to help reduce risks in the responses.
“There have been changes in some of the standards and new guidance from the FDA to enable faster production to open up the supply chain to get more masks and respirators into the market,” Wilson said. “There are still levels of control and risk mitigations strategies that we need to focus on. We’re staying on top of those changes.”
Research on Possible Solutions for Other Shortages
While the face shield is the most mature project the team is developing, researchers are also looking at other needs of the medical community. Among them are ventilators, disinfecting wipes, and respirators.
An example of an Apollo 13 project may be ventilators that are used to help critically ill patients breathe. Traditional equipment makers are working as fast as they can, but that may not be fast enough. To achieve a globally scalable makeshift ventilator will require minimizing the number of parts and thinking about mechanical simplicity, Yee said.
Leon Williams, head of the Centre for Competitive Creative Design at Cranfield University, is working with Georgia Tech researchers to create a makeshift ventilator based on the bag-valve-mask (BVM) – also known as an Ambu bag – a hand-held mechanical resuscitation device already available at hospitals.
Through a system of laser-cut gears and other components, the preliminary concept would use a simple three-volt motor to compress the bag and push air into the lungs of a critically ill patient. Among the challenges is extending the lifetime of the bags, which are not designed for long-term use.
“We need to understand everything about the ventilators that are already in use,” said Susan Margulies, chair of the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University. “By understanding how everything works, we can modify the design to use the components we can get.”
As with face shields, the group expects to make its plans widely available for other groups to iterate and produce. “There is a lot of activity here that is going to move this forward,” said Devesh Ranjan, associate chair for research in the Woodruff School of Mechanical Engineering, who is coordinating several of the Georgia Tech Rapid-Response projects on campus.
Another identified need is for disinfecting wipes, which seem like a simple enough product: a nonwoven material and a solution based on either alcohol or bleach. The material and solutions seem to be available; the problem is locating the industrial-sized containers to hold them.
“We’ve been looking for containers for the wipes commercially,” said Graham. “What we are finding is that the issue is the containers, but we are looking at other solutions.” He’s working with David Sholl, chair of the School of Chemical and Biomolecular Engineering, to identify potential suppliers.
Respirators, Swabs and Gowns
Protecting healthcare workers from the coronavirus requires a special type of respirator, soft face masks that remove virus particles from the air. Because the virus particles are so small, hundreds of nanometers in diameter, that protection requires high-efficiency filtration materials that until recently were mostly manufactured in China.
“The filters are not being produced at the rates that are needed, so we have been thinking about what we can put together that approximates an N95 filter that’s needed to protect healthcare workers,” said Ryan Lively, an associate professor in the School of Chemical and Biomolecular Engineering. “We need to make something that can be produced out of homemade goods, then verify that it can do the filtering needed.”
Lively has been experimenting with alternatives, such as high-efficiency filtration materials manufactured for HVAC systems that could be sewn inside a fabric pouch. “There are journal papers out there showing filtration materials that are not as good as N95 are still effective at increasing rejection of the virus particles,” he said.
If these work as needed, Lively could produce limited numbers in his lab. “We have estimated that we can produce 700 masks per week using the pilot line that we have for research and repurposing it for cranking out hydrophobic fiber media,” he said. “That won’t solve the problem, but it will help meet a very critical need.”
The swabs used for COVID-19 testing are also in short supply, as are gowns designed to protect healthcare workers. Carson Meredith, director of the Renewable Bioproducts Institute, is tracking down alternative sources from among the many manufacturers who are members of the Georgia Tech interdisciplinary research institute.
“The idea is to take a basic material intended for a different function and transform it into the products that we need,” he said. One example is a material manufactured for party tablecloths - plastic on one side to prevent spills from going through, and paper on the other for festive designs. “We’re looking at whether the machinery that produces those can be rapidly turned into making a temporary gown.”
The research team meets by phone daily to update each other on what’s been done and to share ideas. They follow international Slack channels to know what other similar groups are doing across the U.S. and the world.
They know their prototype production equipment can’t meet the world’s needs, so they’re sharing plans with others who may have capabilities. Ultimately, major manufacturers will catch up, but that could take months – perhaps too long for the expected COVID-19 infection curve.
“The best thing we can do is share that information broadly to try to come up with solutions that use parts that can be sourced locally,” Yee said, referring to the ventilator project. “Simple solutions using motors that people can get anywhere, structures that can be 3D-printed and materials that can be hand-cut with saws may get us through this.”
Article updated March 26, 2020
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Contacts: John Toon (404-894-6986) (jtoon@gatech.edu) or Ben Brumfield (404-272-2780) (ben.brumfield@comm.gatech.edu)
Writer: John Toon
Media Contact
John Toon
Research News
(404) 894-6986
Latest BME News
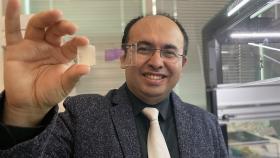
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.