There are a number of factors associated with the prolonged survival of patients with brain cancer. One of the most important involves the amount of tumor that is removed during surgery. There is a fine but critical line between just enough and too much – it’s a delicate and complex balancing act. It is brain surgery, after all.
On the one hand, the patient faces dire results if the tumor isn’t completely resected. On the other, if the surgeon removes normal tissue, it can significantly impair the patients’ motor, sensory, visual, language, and cognitive function. Compounding this complex task is a lack of adequate tools.
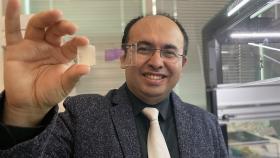
“The main limitations of the current technologies that are available for visualizing tumor margins are that they are expensive, and they’re not accurate or fast enough,” says Francisco Robles, researcher in the Petit Institute for Bioengineering and Bioscience at the Georgia Institute of Technology.
So Robles, an assistant professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University, aims to improve the odds for patients and surgeons by developing a better tool.
“The goal of our work is to lay the foundation for a novel intraoperative tool, based on label-free optical imaging,” explains Robles, whose research recently received an important boost in the form of a three-year, $600,000 R21 grant through the Innovative Molecular Analysis Technologies (IMAT) program, part of the NIH’s National Cancer Institute.
The ideal tool for guiding neurosurgery should clearly differentiate between normal and diseased brain tissue with high subcellular resolution, be fast enough to cover the tumor margin in reasonable time, be cost effective, and be easily integrated into the surgical workflow, providing real-time feedback on a patient who doesn’t have to be moved. Emerging methods have shown promise, but none fill all of these needs.
“Some technologies have difficulty seeing diffusive cells that escape the larger bulk tumor, and so we need higher sensitivity for this,” Robles says. “So our goal is to develop a single tool that allows specificity for individual cells that are cancerous, while having the speed to see large volumes in reasonable time.”
Blending People and Tech
His proposed method is based on new optical technology that leverages two complimentary, label-free molecular imaging methods: stimulated Raman scattering (SRS) and spectroscopic optical coherence tomography (SOCT). SRS provides rich molecular information with high subcellular, or spatial, resolution, but it is unable to cover large areas at high speeds. Meanwhile, SOCT can multiplex both the special and spectral information to achieve high-speed, tomographic molecular imaging (but has limited molecular sensitivity).
“We want to merge both of those worlds,” says Robles, whose multidisciplinary, collaborative SRS-SOCT approach addresses limitations of each individual method, exhibiting additional capabilities that improve the ability to identify brain tumors.
Robles plans to develop an improved SRS-SOCT system through a partnership with Harald Giessen at the University of Suttgart, then test the technology in collaboration with Emory neurosurgeon Jeffrey Olson, and finally, validate SRS-SOCT for identifying brain tumors in humans using specimens obtained through the Human Tissue Procurement Service at Emory’s Winship Cancer Institute.
“This work will pave the way for a novel intraoperative tool that has the potential to increase the success rate of neurosurgery,” says Robles, “and prolong survival for patients with malignant brain tumors.”
Media Contact
Jerry Grillo
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.