Four Coulter BME research groups will offer more details alongside deeper discussions at Symposium on Health Disparities
By Jerry Grillo
Alopecia was front and center for Valencia Watson long before Academy Award winner Will Smith and comedian Chris Rock made it topical with the smack seen round the world.
A third-year graduate student in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University, Watson struggles with a form of the autoimmune disease, which causes hair loss and is two to six times more prevalent in Black women, like her, than in other people.
Personal experience drove her to study the mechanisms underlying alopecia, and in so doing, Watson has inspired a new project and focus area in the lab of Coulter BME Professor Cheng Zhu. It’s one of four early-stage projects launched by the Department last year aimed at developing new tools for studying diseases that disproportionately affect people of African descent.
Ultimately, the research teams hope to develop animal models that will more closely replicate the risk factors and social determinants of health common among Black Americans. Each received a $25,000 seed grant, “to get us started in applying our expertise to address a very big challenge,” said Ed Botchwey, who developed the program with fellow Coulter BME faculty member Johnna Temenoff.
“Developing these systems that can model the underlying causes of health disparities will eventually allow us to bring the different aspects of biomedical engineering to bear,” added Botchwey, an associate professor. “I’m looking forward to seeing how the seed grant support has impacted these researchers and what they’ve been able to do so far.”
Botchwey will get his chance April 18 at the Symposium on Health Disparities, when the four research teams will present their work so far. The event also will include the Academy of Medicine Distinguished Lecture from University of Connecticut Professor Cato Laurencin, who basically launched the field of regenerative engineering. He’ll talk more about diminishing racial disparities in healthcare and biomedical research.
“He’s the consummate physician-scientist,” Botchwey said. “I think he’ll address the efforts we can make to not only impact health disparities but perhaps also what so many of us were desperate for during the season of protest: making real progress in the area of racial equity. He’ll speak powerfully to that, and we’ll hear his perspective on the challenges in front of us.”
But first, attendees will be briefed on the challenges that the four Coulter Department research teams are tackling right now:
Alopecia Areata
Cheng Zhu, principal investigator; Loren Krueger, Emory University, co-investigator
Alopecia is an autoimmune disorder in which T cells mistakenly attack hair follicles, and to develop a better disease model, Zhu’s team has to figure out why. Zhu credited Watson with moving the lab in this direction.
“Valencia convinced us,” said Zhu, Regents Professor and J. Erskine Love Chair in Engineering in the Coulter Department. His lab studies how immune cells sense, respond to, and adapt in a dynamic environment while being buffeted by natural mechanical forces in the body.
“We’ve used our approach to study T cells in tumor immunology [and] infection, but not autoimmune diseases,” Zhu said. “So we think it’s a good idea to include alopecia areata, because it’s one of the most prevalent autoimmune disorders in the world.”
Watson said she wasn’t totally convinced that her condition was an autoimmune disorder at first, because there is no evident antigen activity to incite the T cells. That’s given the research team something to look for. Watson sees it as, “an opportunity to contribute to the research by first identifying what is activating the T cells.”
Their work to this point has manifested in a perspective article, with Watson and fellow grad student Makala Faniel as lead authors, discussing the potential for mechanobiology and mechanoimmunology “to contribute to alopecia research by adding new methods, new approaches, and new ways of thinking,” they wrote.
Breast Cancer
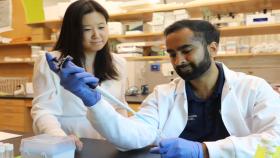
Karmella Haynes, principal investigator; Curtis Henry, Emory University, co-investigator
When the seed grant program was announced, Haynes’ lab was already at work developing an engineered protein to activate genes that are silenced in triple negative breast cancer cells, and she was working with Henry’s lab on developing epigenetics experiments for another type of cancer, acute lymphoblastic leukemia.
“Dr. Henry had done some exciting work showing how obese-associated serum affected epigenetics and gene expression,” said Haynes, an assistant professor. “We started thinking about how to translate this research to triple negative breast cancer, which disproportionately kills African American women.”
They are two very different forms of cancer, but their project is investigating how the biochemistry of serum in obese patients might affect epigenetic states in breast cancer, and make the disease more aggressive and deadly.
“Once we understand this, we can artificially reprogram the epigenetic state and block cancer cell replication and the formation of new tumors in other parts of the body,” Haynes said.
Led by postdoctoral fellow Cara Shields, the Haynes lab will share new data at the symposium, showing how fat cells can actually prevent cancer cell death by silencing the genes that would otherwise activate a suicide switch or prevent the cancer from spreading.
While they haven’t created the animal model that replicates these conditions yet, Haynes and her collaborators are currently applying for a major external grant and plan to publish their results. First, they want to complete their investigation of gene silencing and demonstrate how epigenetic engineering can be used to activate the affected genes.
“We are working on making our approach, ‘epigenome actuation,’ more clinically translatable to cancer and generally applicable to other diseases that affect cell development,” Haynes said.
Glaucoma
C. Ross Ethier, principal investigator; Michael Anderson, University of Iowa, and Michael Hauser, Duke University, are collaborators
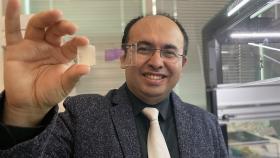
Black people are three to four times more likely to develop glaucoma than people of Asian or European descent, and it progresses faster: People of African descent are six times more likely to go blind. Cydney Wong, a Ph.D. student who has taken the lead on this research in the Ethier lab, knows this all too well.
“My grandmother, who I grew up with, has glaucoma, so I have a personal interest in this disease,” Wong said. “I’ve watched as her vision gradually declined. At this point she is almost completely blind.”
Her grandmother is 90 and loves hearing about Wong’s research, which is now focused on a certain genetic risk factor associated with people of African descent all over the globe.
“Our project is investigating whether a mouse expressing this genetic risk factor exhibits glaucomatous damage in its eye,” Wong said. “However, I think the more big-picture goal would be to better understand why glaucoma tends to progress so quickly in people of African descent so that we can develop treatments to prevent vision loss in these patients.”
Traumatic Brain Injury
Michelle LaPlaca, principal investigator; Levi Wood, mechanical engineering, Georgia Tech, co-investigator
LaPlaca has spent the better part of her career studying traumatic brain injury (TBI) from multiple angles, to understand the underlying mechanisms during and following an injury. The idea is to develop better strategies for diagnosis and treatment.
With this project, she’s also attempting to probe the risk factors that can make TBI worse, to gain a deeper understanding of why some underrepresented groups, such as African Americans, with TBI are significantly more likely to have post-injury complications.
LaPlaca’s team is piecing together how chronic stressors and dietary factors, which have not been applied together for the study of TBI animal models before, may influence outcomes.
“I’ve been very interested in the heterogeneous factors that contribute to traumatic brain injury complications,” said LaPlaca, who was inspired somewhat by a meeting of the National Neurotrauma Society last year. “We held a session for the first time on health disparities in TBI, in which we discussed rural-urban disparities, race disparities, and social determinants. It was very timely and re-energized my interest in this area of research.”
Basically, her team is working to develop a state of stress before injury, “a new direction for me,” LaPlaca said. “But I think it’s really critical that we start to use some of these more complicated models in our animal research to complement clinical and public health efforts.”
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.