Last year, commercial medical history was made when the Food and Drug Administration (FDA) approved the first gene therapy treatment, Kymriah, in the U.S., opening the door to a new world of treatment for devastating diseases. As reports from clinical trials of tisagenlecleucel (marketed as Kymriah) became public – that it used a patient’s own T-cells to actually kill cancer – the news media called it a miracle cure.
Of course, it took decades of research, a lot of trial and error at the molecular level. The concept, transplanting normal or healthy genes into cells in place of missing or defective genes in order to treat diseases and disorders, has been under development since the Reagan administration.
“The idea of gene therapy’s been around since I was a kid,” says Wilbur Lam, associate professor in the Wallace H. Coulter Department of Biomedical Engineering at Emory University and the Georgia Institute of Technology and researcher in the Petit Institute for Bioengineering and Bioscience at Georgia Tech. “In the 1990s, gene therapy trials mostly failed and often caused deadly side effects like cancer. But the entire field has moved forward, and the field of gene therapy has now learned how to actually cure people.”
As it turns out, miracles are not only complex and elusive, they’re also expensive, to the point of being infeasible for large scale clinical translation. But with support from a new R01 grant from the National Institutes of Health (NIH), Lam’s lab is working to make gene therapies more efficient, and more economically accessible.
Kymriah, for example, has a price tag of $475,000 (or about $20,000 less than the value of Lam’s new four-year NIH grant).
“That price tag is largely a result of the difficulty and cost associated with viral vector manufacturing, which is, unfortunately, the key to these novel therapies,” says Reginald Tran, a postdoctoral researcher in Lam’s lab who is using microfluidic technology that he developed to incorporate basic mass transfer and fluid mechanics principles to increase gene therapy efficiency.
In gene therapy modified viruses often are used as vectors, or vehicles, to carry the good-guy genes into a human cell. It’s been proven to work, but it’s not a very efficient process, according to Lam. For one thing, “it takes about a billion cells to treat an adult for something like sickle cell disease,” he says.
Also, Lam notes that these engineered viral vectors have a half-life, “and they’ll deactivate if they don’t find their target cell in time. They will die. Excess virus is given to cells to ensure that enough cells get genetically modified, but this results in added costs and significant waste of the precious key reagent. ”
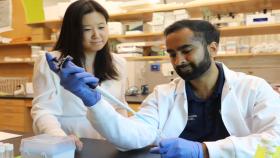
Tran, who earned his Ph.D. in the Lam lab, says he was amazed to learn about the capabilities of microfluidics, and how leveraging the differences in physics at the micro scale could unlock new possibilities for diagnostics and therapeutics.
“This project was really ideal for me since I could combine my backgrounds in mechanical engineering and microfluidics toward gene and cell therapy,” Tran adds. “I quickly found that microfluidics were the perfect platform to efficiently bring cells and viral vectors together to maximize gene transfer.”
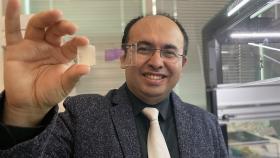
Performing the critical gene transfer step in microfluidics dramatically reduces processing time and resources (up to five times less viral vector can be used). While many researchers continue to work on developing more potent genes or increasing viral vector manufacturing potential, the Lam group is focused on using less virus.
“At a time when virus shortages present a huge bottleneck in gene and cell therapy commercialization, we believe that our technology can help make these treatments more accessible and affordable for patients,” Tran says. “I feel extremely lucky to work on a problem that has the potential to make a meaningful impact on what could very well be the next frontier in modern medicine.”
Media Contact
Jerry Grillo
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience
Keywords
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.